Lung Transplantation: Survival Rates, Procedure, Recovery, and Eligibility Criteria
1. Introduction to Lung Transplantation
Lung Transplantation: Survival Rates, Procedure, Recovery, and Eligibility Criteria: The decision to undergo lung transplant surgery is made when patients face a poor prognosis due to lung failure caused by conditions such as chronic obstructive pulmonary disease (COPD), idiopathic pulmonary fibrosis (IPF), or cystic fibrosis (CF). This article will cover everything from lung transplant eligibility criteria to post-lung transplant care and complications.
2. Understanding Lung Transplantation
The lung transplant procedure involves replacing one or both of the patient’s diseased lungs with those from a healthy donor. Double lung transplant vs single lung transplant is a common decision point, with doctors assessing which option best suits the patient’s needs.
How long does it take to recover from a lung transplant? Recovery can vary, but lung transplant recovery timeline generally spans several months of intense rehabilitation, which includes regular monitoring for signs of lung transplant rejection and infections.
3. Indications for Lung Transplantation
Lung transplantation is typically indicated when lung diseases reach an end-stage where the patient’s lungs can no longer function properly. Some of the most common conditions that lead to the need for a lung transplant include:
- Chronic obstructive pulmonary disease (COPD): A leading cause of lung transplant surgery in the elderly.
- Idiopathic pulmonary fibrosis (IPF): A progressive lung disease that causes scarring of lung tissue and may require lung transplant procedure.
- Cystic fibrosis (CF): A genetic disorder often resulting in the need for a lung transplant due to irreversible lung damage.
- Pulmonary hypertension: High blood pressure in the lungs, which can also lead to the need for lung transplant surgery.
Lung transplant eligibility criteria require patients to be assessed for their overall health, lung function, and willingness to undergo the demanding process of recovery.
Symptoms Leading to Lung Transplantation: A Critical Guide
When symptoms of lung failure worsen, it becomes imperative to consider lung transplantation as a viable treatment option. Lung transplantation is often a life-saving procedure for patients whose lung function has deteriorated to the point where other treatments can no longer provide adequate relief. Below are some of the key symptoms that may indicate the need for a lung transplant:
1. Shortness of Breath with Minimal Exertion
As lung function declines, individuals may experience shortness of breath even with simple tasks such as walking short distances, climbing stairs, or performing daily activities. This is one of the most common symptoms indicating that the lungs are no longer able to supply the body with enough oxygen, signaling the need for urgent medical evaluation.
2. Chronic Cough that Doesn’t Respond to Usual Treatments
A persistent cough that does not improve despite using standard medications or treatments could be a sign of significant lung damage. It may be the result of a chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, or another condition that causes irreversible damage to lung tissue.
3. Fatigue and Overall Weakness
People with severe lung failure often experience constant fatigue and weakness. This occurs because the body is not getting enough oxygen, causing a lack of energy and an overall feeling of exhaustion. Patients may find it challenging to perform even simple tasks due to this debilitating weakness.
4. Hypoxemia (Low Blood Oxygen Levels)
Hypoxemia refers to dangerously low levels of oxygen in the blood. This condition is often diagnosed through blood tests or pulse oximetry and may be accompanied by symptoms such as confusion, rapid heart rate, and bluish skin color (cyanosis). Hypoxemia is a serious sign that lung function is significantly impaired and can lead to organ damage without appropriate intervention.
5. Other Symptoms to Watch Out For
- Frequent respiratory infections: Chronic lung conditions may predispose individuals to infections, leading to frequent hospitalizations.
- Weight loss: Severe lung disease can cause unintentional weight loss due to difficulty breathing and a lack of appetite.
- Swelling in the legs or abdomen: Fluid retention caused by heart failure or lung problems may lead to swelling, indicating worsening heart or lung function.
Early Recognition and Timely Intervention
Recognizing these symptoms early and seeking timely medical intervention is crucial for patients experiencing lung failure. A thorough evaluation by a pulmonologist will help determine whether the patient is a candidate for lung transplantation. Medical teams assess lung function, oxygen levels, overall health, and the underlying condition causing lung failure before making the decision.
Eligibility Criteria for Lung Transplantation
Not all patients experiencing symptoms of lung failure are eligible for a lung transplant. Some of the factors considered include:
- Age and overall health
- The cause of the lung disease
- The severity of symptoms and the impact on quality of life
- Whether other treatments have been ineffective
- The absence of other serious medical conditions
Lung transplantation is not a cure, but it can significantly improve quality of life and increase life expectancy for those with end-stage lung disease. It is important to work closely with a healthcare team to understand the benefits, risks, and potential outcomes of lung transplantation.
5. Causes of Lung Failure
Lung failure can result from many conditions, some of which are preventable. Common causes include:
- Environmental factors, like air pollution, contribute to chronic lung diseases such as COPD, which may ultimately require lung transplant surgery.
- Genetic disorders, such as cystic fibrosis or alpha-1 antitrypsin deficiency, are significant contributors to severe lung disease.
- Infections, such as pneumonia, can lead to irreversible lung damage, making lung transplantation the only viable option for some patients.
Understanding the cause of lung disease leading to transplant eligibility is essential for doctors in determining the best course of action, including evaluating for lung transplant surgery.
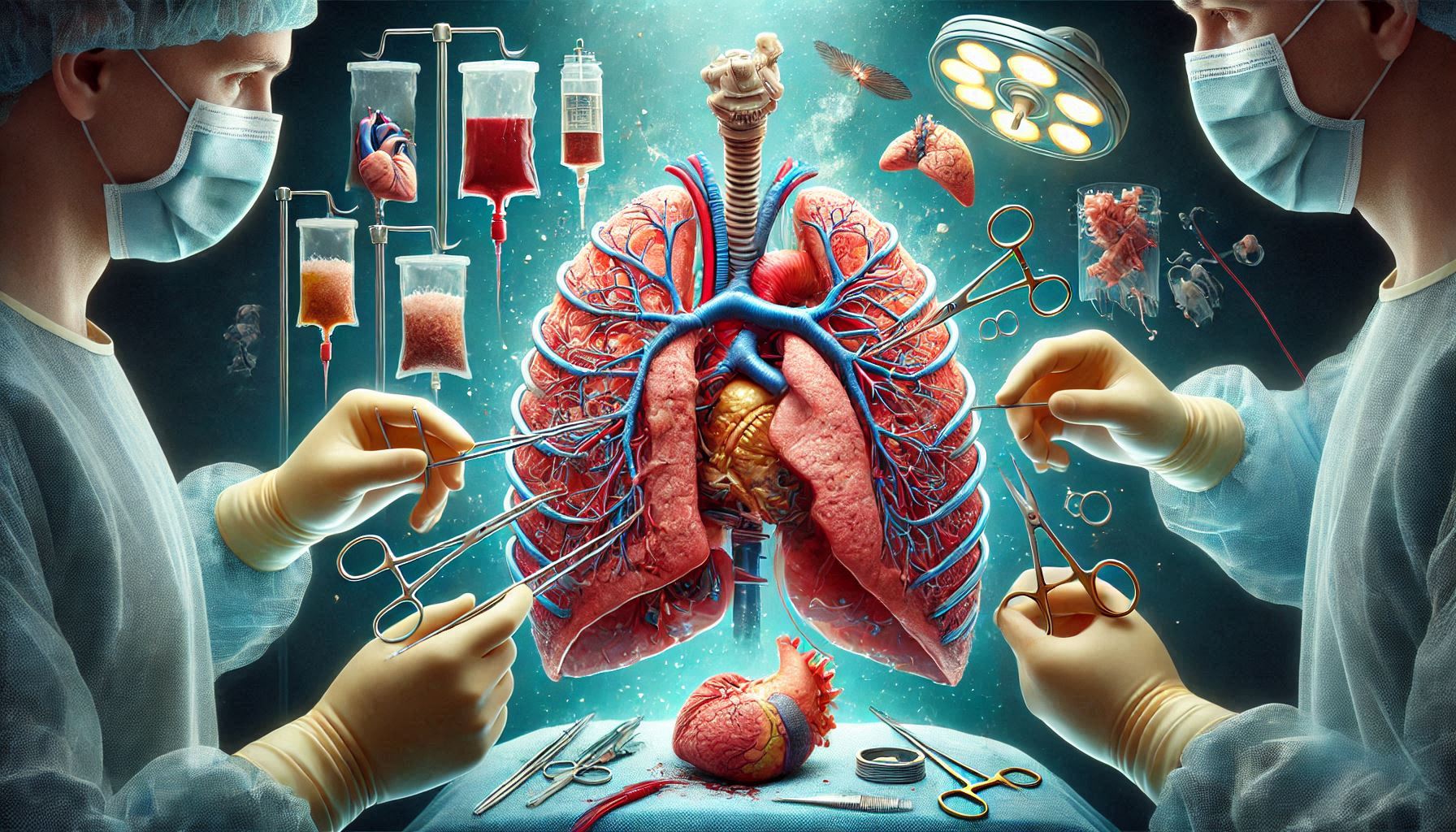
6. Lung Transplantation Procedure
Before a lung transplant, patients must undergo a thorough evaluation to ensure that they are suitable candidates for the procedure. Key steps in the lung transplant procedure include:
- Imaging tests like CT scans to assess the degree of lung damage.
- Pulmonary function tests to determine how well the patient’s lungs are functioning.
- Blood tests to check for infections and organ compatibility.
- Psychosocial evaluations to ensure the patient is prepared for the emotional and mental challenges post-transplant.
Once a patient is approved and placed on the lung transplant waiting list, the matching process begins, considering factors like blood type and lung size. Donor lungs are matched with patients according to these factors, which can affect the lung transplant procedure.
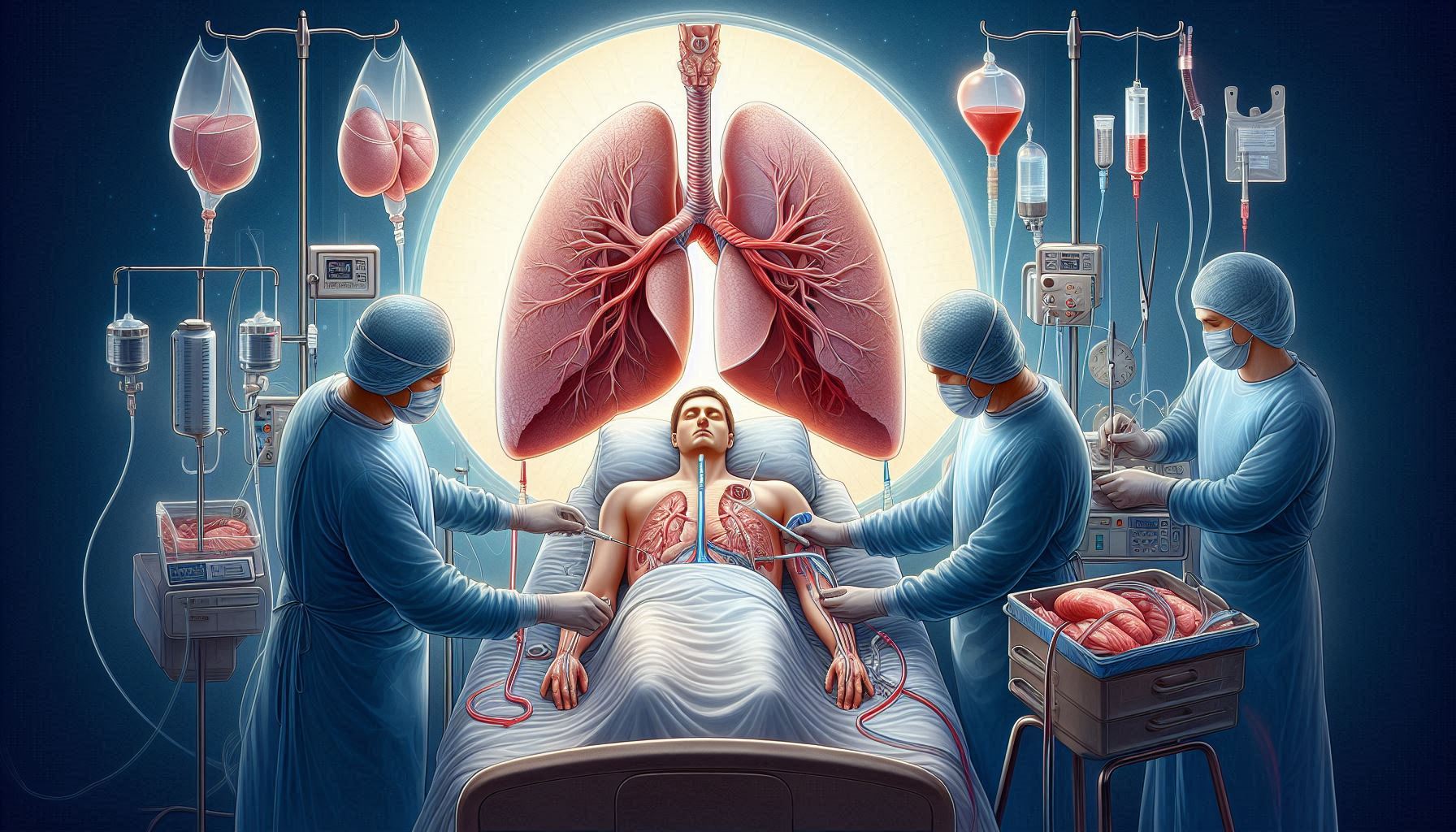
7. Post-Transplantation Care and Treatment
After a lung transplant, patients must adhere to strict guidelines to ensure a successful recovery. Important aspects of post-lung transplant care include:
- Immunosuppressive therapy to prevent the immune system from rejecting the new lungs.
- Infection prevention, as lung transplant patients are at high risk due to immunosuppressive drugs.
- Regular monitoring for signs of lung transplant rejection, including chest biopsies and tests of lung function.
- Rehabilitation to help patients regain strength and lung capacity, especially in the early months following surgery.
Adhering to these protocols is critical to ensure that patients maintain a healthy lung function after lung transplantation.
Challenges and Complications of Lung Transplantation
Lung transplantation, though a life-saving procedure, comes with its own set of challenges and potential complications. It is crucial for both patients and healthcare providers to understand these risks, as proper management can significantly influence the outcome of the transplant. The primary complications include rejection, infections, chronic rejection, and cancer, all of which can affect the success and longevity of the transplanted lung. Below, we delve deeper into each of these challenges:
1. Rejection: The Immune System Attacks the New Lungs
One of the most significant risks following lung transplantation is rejection, where the body’s immune system identifies the new lungs as foreign tissue and attacks them. This occurs because the immune system recognizes the donor lung as different from the recipient’s tissue, triggering an immune response. There are three types of rejection:
- Hyperacute rejection: This occurs immediately after surgery, typically within hours, and is due to a pre-existing antibody reaction. It is very rare and often leads to the immediate failure of the transplant.
- Acute rejection: This is more common and typically happens within the first few months after the transplant. It occurs when the immune system reacts to the donor lung, causing inflammation and potential damage to the tissue.
- Chronic rejection: This type of rejection develops over the long term and causes progressive damage to the transplanted lung, leading to a decline in lung function. Chronic rejection is one of the leading causes of failure in lung transplants.
Managing rejection involves administering immunosuppressive medications, which lower the immune system’s ability to attack the transplanted lung. However, these medications need to be carefully managed to avoid infection and cancer, which are other risks.
2. Infections: A Common Risk for Post-Transplant Patients
After a lung transplant, the patient’s immune system is intentionally suppressed to prevent rejection. However, this makes lung transplant patients more vulnerable to infections, which can severely affect the outcome of the surgery. Infections may arise from several sources:
- Bacterial infections: These are common, especially respiratory infections, such as pneumonia, which can be very serious post-transplant.
- Viral infections: The patient may be susceptible to viruses like cytomegalovirus (CMV), which can lead to severe complications if left untreated.
- Fungal infections: Fungi, such as aspergillus, are also a risk, particularly in patients with weakened immune systems.
Patients must undergo continuous monitoring for signs of infection, and treatment typically involves a combination of antibiotics, antifungals, and antivirals. Early detection and treatment are critical to preventing infections from escalating into life-threatening complications.
3. Chronic Rejection: Long-Term Damage to the Transplanted Lung
Chronic rejection is a gradual and ongoing process where the immune system continues to damage the transplanted lung over time. Unlike acute rejection, which is typically reversible with treatment, chronic rejection leads to irreversible scarring of the lung tissue. This results in a condition known as bronchiolitis obliterans syndrome (BOS), which is characterized by:
- Progressive shortness of breath
- Decreased lung function
- Chronic cough and wheezing
The exact cause of chronic rejection is not fully understood, but it is believed to involve a combination of immune response, environmental factors, and other pre-existing conditions in the patient. Chronic rejection is one of the primary causes of lung transplant failure and often leads to the need for a second transplant. The condition is managed with medications and close monitoring of lung function, but it remains a significant challenge in long-term lung transplant care.
4. Cancer: Increased Risk Due to Immunosuppressive Medications
While immunosuppressive medications are crucial in preventing rejection, they also increase the risk of cancer in lung transplant recipients. These medications work by suppressing the immune system, which makes it less effective in detecting and destroying abnormal cells that could lead to cancer. The types of cancer most commonly associated with immunosuppressive therapy include:
- Skin cancer: Due to the weakened immune system, patients are at a higher risk of developing skin cancers, particularly non-melanoma skin cancers such as basal cell carcinoma and squamous cell carcinoma.
- Lymphoma: A type of cancer that affects the lymphatic system, lymphoma is more common in transplant recipients due to the effects of immunosuppressants.
- Kaposi’s sarcoma: This rare type of cancer is linked to infections caused by certain viruses, and transplant recipients may be more vulnerable due to their suppressed immune systems.
To mitigate this risk, lung transplant patients are regularly monitored for signs of cancer, and preventive measures such as using sunscreen, avoiding tanning beds, and limiting sun exposure are recommended. Additionally, a strong follow-up care program is necessary to detect early signs of cancer so that it can be treated before it progresses.
5. Managing the Risks: Medication and Regular Monitoring
The key to successfully managing these risks lies in a combination of appropriate medications, close monitoring, and lifestyle changes. Here’s how each of these factors contributes to improving the patient’s long-term success:
- Immunosuppressive medications: These are critical for preventing rejection, but they need to be carefully managed. Over-suppression can lead to infections and cancer, while under-suppression can result in acute rejection.
- Infection prevention: Patients are typically placed on prophylactic medications to reduce the risk of infections. Regular check-ups and screenings are essential to catch infections early before they cause major complications.
- Cancer surveillance: Regular skin checks and other screenings are necessary to identify and treat cancer early. This also includes regular follow-ups to ensure the patient is maintaining a healthy lifestyle and staying protected from environmental risks.
- Regular lung function tests: Pulmonary function tests are key to assessing lung transplant survival rates and detecting issues like chronic rejection or declining lung function.
While lung transplantation offers hope to patients with severe lung disease, it is not without its risks. Rejection, infections, chronic rejection, and cancer are all potential complications that must be managed with close monitoring and careful medication management. Understanding these risks and being proactive in their management is essential for improving the chances of success and extending the life of the transplanted lungs.
By taking a holistic approach—incorporating regular medical check-ups, effective medication management, and lifestyle adjustments—lung transplant patients can navigate these challenges and increase their chances of a positive outcome. As medical advancements continue, the long-term success of lung transplantation is likely to improve, offering better survival rates and quality of life for recipients.
9. Advances in Lung Transplantation
The field of lung transplantation has seen major advances in both surgical techniques and post-operative care. These innovations include:
- Minimally invasive lung transplant techniques, which reduce recovery time and surgical risks.
- Stem cell research in lung transplantation, which may offer a promising future for regenerating damaged lung tissue and reducing the need for organ donors.
- Xenotransplantation, where researchers explore using animal organs, like pig lungs, for human transplantation to alleviate organ shortages.
Such innovations may help improve lung transplant survival rates and reduce complications in the future.
10. Conclusion
Lung transplantation is a complex, life-changing procedure that can offer a new lease on life for individuals suffering from end-stage lung disease. Lung transplant survival rates have improved significantly thanks to advances in medical science, surgical techniques, and post-transplant care. However, it is important for patients to carefully consider their lung transplant eligibility criteria, the risks involved, and their commitment to the post-surgery recovery process.
If you or a loved one is considering lung transplant surgery, it’s essential to seek out top-rated hospitals for lung transplants and discuss the potential benefits, risks, and long-term outcomes with your healthcare provider. Understanding the lung transplant procedure, immunosuppressive therapy, and post-surgery care will help you navigate the road to recovery and ensure the best possible outcome.